What Does Clay Stool Look Like?
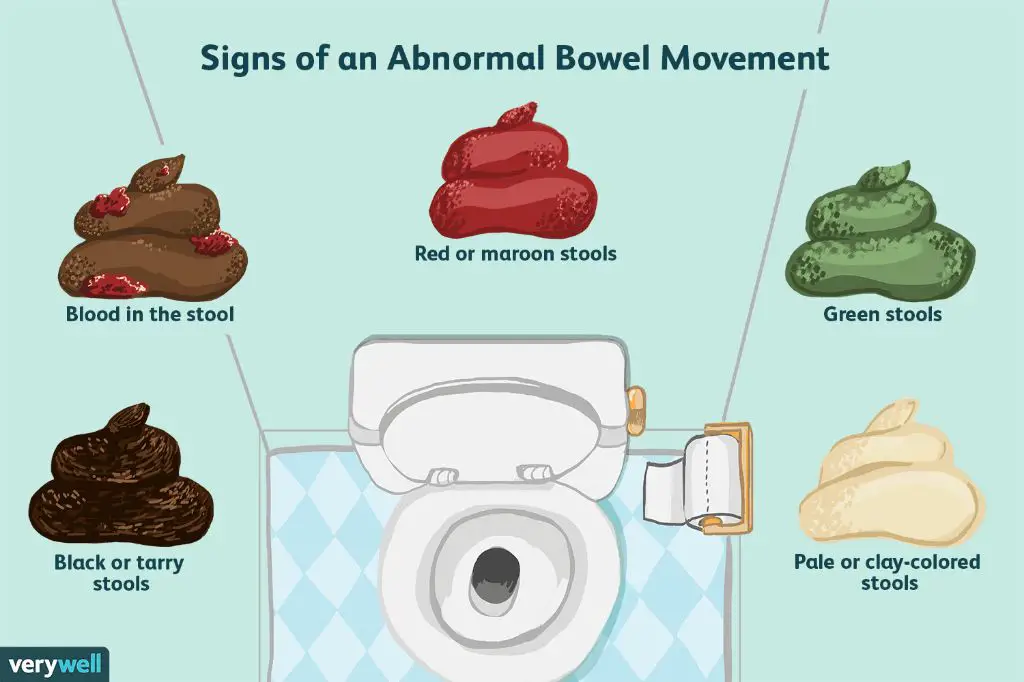
Clay-colored stool refers to pale, clay-like poop that is light in color. The normal brown color of stool comes from bile, which is produced in the liver and secreted into the small intestine. When stool lacks this typical brown color, it often means that bile is absent. The lack of bile can make stool appear white, gray, or pale yellow – a clay-like color.
Clay-colored stool is typically a sign of a problem with bile flow, such as from reduced production or obstructed bile ducts. It can indicate liver diseases like hepatitis or cirrhosis, as well as gallbladder conditions like cholecystitis and gallstones. Symptoms that may accompany clay-colored stool include itching, abdominal discomfort, fatigue, and jaundice.
Appearance
Clay-colored stool has a pale, clay-like appearance. The normal brown color of stool comes from the interaction between bilirubin and bile salts released by the liver during digestion. In clay-colored stool, this process gets disrupted, resulting in pale or gray colored stool the color of clay. The texture of clay-colored stool is generally soft or loose rather than formed or hard. The shape may appear narrow, thin, or pencil-like. Clay-colored stool typically has little or no discernible odor.
In contrast, normal healthy stool is shades of medium or dark brown and has a soft to firm, sausage-shaped appearance. The surface may show cracks or lumps from the contraction of the intestine during transit. Normal stool generally has a mild odor that is not overly foul or unusual.
If stool appears pale, dry, loose, and foul-smelling, it could indicate an underlying condition disrupting the digestive process (source). Consulting a doctor is recommended to determine the cause.
Causes
Some common causes of clay-colored stool include:
- Gallbladder or liver disease – Conditions like cholecystitis, cirrhosis, hepatitis, and gallstones can lead to reduced bile output, resulting in pale stools. [1]
- Gastrointestinal infection – Infections from bacteria, viruses, or parasites can affect the gastrointestinal tract and lead to pale stool. Common infections include giardia and c. difficile. [2]
- Bile duct obstruction – Tumors, cysts, or gallstones blocking the bile ducts prevent bile from reaching the intestines, causing clay-colored stool. [3]
- Pancreatic insufficiency – Diseases like pancreatic cancer, cystic fibrosis, and chronic pancreatitis can reduce pancreatic enzyme output, affecting digestion and stool color.
- Celiac disease – Malabsorption from celiac disease prevents proper breakdown and absorption of fat, causing pale stool.
Clay-colored stool is often indicative of an underlying issue preventing bile release or production, rather than an isolated condition itself. Seeking medical evaluation can determine the specific cause.
Diagnosis
Doctors typically diagnose clay-colored stool through a physical exam and questions about your symptoms. They will look for signs of jaundice, tenderness in the abdomen, or an enlarged liver or spleen that could indicate an underlying condition. Stool sample tests are often used to help confirm a diagnosis.
A fecal occult blood test checks the stool for traces of blood that are not visible to the naked eye. This can identify potential sources of bleeding in the digestive tract like ulcers, polyps, or cancer.
A fecal fat test checks how well your body is absorbing and digesting fat. High levels of fat in stool can indicate diseases of the pancreas, liver, or small intestine.
An ova and parasite test looks for parasites or eggs in the stool that could be causing gastrointestinal symptoms and abnormal stool.
A stool culture can identify bacteria, viruses, or other pathogens that are causing an infection in the digestive system.
Imaging tests like an abdominal ultrasound, CT scan, or MRI allow doctors to visually inspect the liver, gallbladder, and pancreas for abnormalities that could be contributing to pale stool.
Blood tests can also help reveal problems with liver enzymes or bilirubin levels that signal liver or bile duct disease (source: https://www.healthline.com/health/stools-pale-or-clay-colored).
Treatment
Treatment for clay-colored stool depends on the underlying cause. If the pale stool is due to a blocked bile duct, surgery may be needed to unblock it. Medications like ursodeoxycholic acid can help regulate bile flow. If infections are the cause, antibiotics can treat bacterial infections while anti-parasitics treat parasites. For people with cirrhosis, treatment focuses on managing the condition. If gallstones are present, the gallbladder may need to be removed. When certain supplements or medications lead to pale stool, stopping them may resolve symptoms. Eating more colorful fruits and vegetables can also help by adding color back into pale stools.
Overall, identifying and addressing the root cause is key to resolving clay-colored stools. This may involve imaging tests, bloodwork, and consulting specialists like gastroenterologists to pinpoint the issue. Treatment can range from simple dietary changes to medications or procedures. The goal is to restore normal digestion and bowel function. With proper treatment guided by a doctor, the outlook is often good.
Lifestyle Changes
Making certain lifestyle modifications may help manage conditions causing clay-colored stool. Focusing on dietary changes, probiotic intake, and hydration can be beneficial.
Eating more fiber-rich foods like fruits, vegetables, whole grains, beans, and legumes can add bulk to stool and promote regular bowel movements. Increasing fiber intake should be done gradually to avoid gas or bloating. Drinking more fluids is also recommended when boosting fiber intake (Health.com).
Taking probiotic supplements containing healthy gut bacteria may help restore normal bowel function and stool consistency. Probiotics can be found in capsule form or in fermented foods like yogurt, kefir, sauerkraut, and kimchi. Consulting a doctor before starting probiotic therapy is recommended (Medical News Today).
Staying hydrated by drinking adequate water and fluids can soften stool and prevent constipation. The recommended daily fluid intake is around 2 liters for women and 3 liters for men. However, needs vary depending on factors like activity level, climate, and health conditions (The Healthy).
Home Remedies
There are some natural home remedies that may help manage the symptoms of clay-colored stool and support liver health. However, these should not replace medical treatment if a serious underlying condition is causing your symptoms.
Some potential home remedies include:
- Drinking bone broth, which can help repair the gut lining and provide electrolytes. Bone broth is made by simmering animal bones and connective tissue in water for several hours to extract the nutrients. Chicken or beef bones work well.
- Eating unsweetened applesauce, which provides pectin to help firm up loose stools. Applesauce is a good source of nutrients and easy for the body to digest.
- Trying digestive bitters before meals, which can stimulate bile production and improve digestion. Look for bitters containing gentian, dandelion, or artichoke.
- Drinking vegetable juice and eating greens to increase fiber intake. Getting more fiber from fruits, vegetables, whole grains and legumes can help regulate bowel movements.
- Taking milk thistle supplements, which have antioxidant and anti-inflammatory properties that support liver health. Speak to your doctor before starting any new supplements.
It’s important to stay hydrated by drinking plenty of water when experiencing clay-colored stool. Proper hydration can help prevent electrolyte imbalances. Avoid alcohol, fatty foods, and NSAIDs during this time. See your doctor if home remedies do not resolve your symptoms.
Complications
Clay-colored stool can potentially lead to complications like dehydration and malnutrition if the underlying condition is left untreated (Medical News Today). Dehydration occurs when the body loses more fluid than it takes in, resulting in an imbalance of water and electrolytes. This can happen with prolonged diarrhea or vomiting which sometimes accompanies conditions that cause pale stool. Dehydration can lead to dizziness, increased heart rate, fever, and confusion if severe. Malnutrition refers to a deficiency in overall calories, protein, vitamins or minerals needed for the body to function optimally. It can occur over time when digestive conditions like cholestasis or pancreatic problems inhibit the body’s ability to properly digest and absorb nutrients from food. Symptoms may include unintentional weight loss, loss of appetite, muscle wasting, and general weakness. Seeking prompt medical treatment for the underlying cause of clay-colored stool can help prevent these potential complications from worsening.
When to See a Doctor
Clay-colored or pale stools can often be caused by lifestyle factors or temporary conditions, but prolonged symptoms should prompt a visit to your doctor. You should schedule an appointment if you experience persistent pale stool along with any of the following warning signs:
- Diarrhea lasting more than 2-3 days
- Unexplained weight loss
- Severe abdominal pain or cramping
- Nausea or vomiting
- Fever or chills
- Blood in stool
- Dark urine
- Yellowing skin or eyes (jaundice)
These symptoms, especially when occurring together, can indicate an underlying liver, gallbladder, or pancreatic disorder that requires medical attention. Prompt diagnosis and treatment is important to prevent complications and restore normal digestive health.
Even if you don’t have additional symptoms, pale stool that persists more than 3-4 days warrants a doctor’s visit for evaluation. Your doctor can run tests to pinpoint the cause, such as bloodwork, stool analysis, imaging scans, or endoscopy procedures. Based on the results, appropriate treatment can be determined.
Don’t hesitate to see a gastroenterologist if your pale stools do not resolve on their own. With proper diagnosis and care, most causes of clay-colored stool can be successfully managed.
Conclusion
In summary, clay-colored stool that looks pale or gray can indicate a potential health problem with bile flow or digestion. Some common causes are gallstones, infections, medication side effects, and pancreatic issues. While lifestyle changes like eating more fiber may help manage mild cases, it’s important to consult a doctor for an accurate diagnosis and proper treatment. They can run tests to determine the underlying cause and recommend treatment options like medication or surgery. Don’t try to self-diagnose or self-treat persistently discolored stool. Seeking timely medical care can prevent complications or serious conditions from worsening.